Connaître son Nembutal,Non classé
What is Nembutal used for ?
Pentobarbital is primarily used for emergency seizure control (status epilepticus), inducing therapeutic comas in brain injury patients, procedural sedation, veterinary anesthesia and euthanasia, and in jurisdictions where legal, for medical aid in dying and capital punishment.
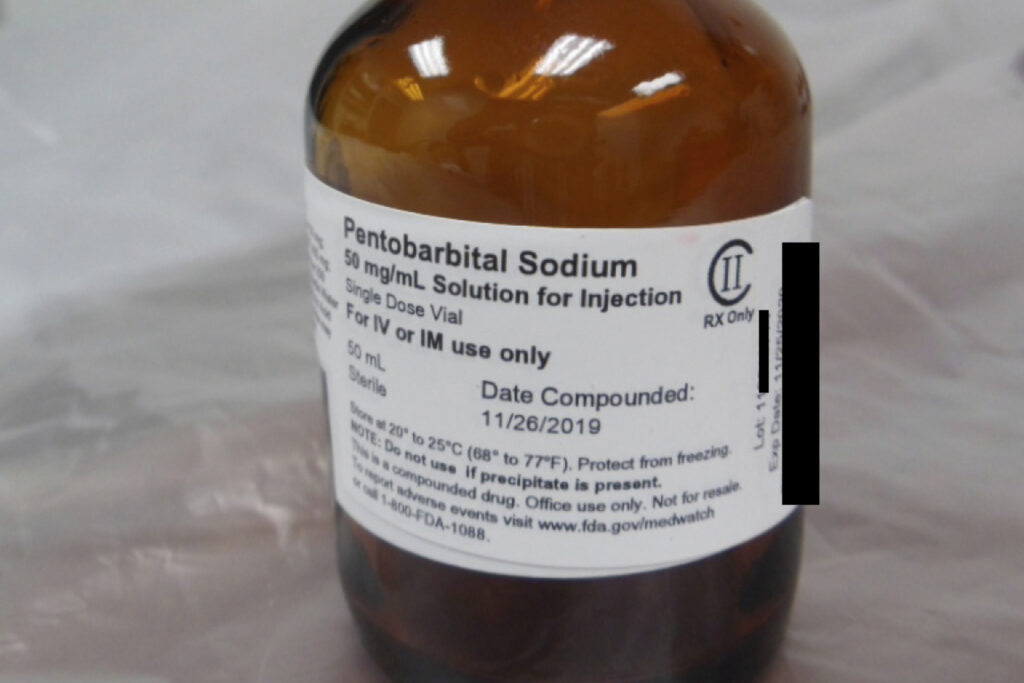
Pentobarbital, commercially known by the brand name Nembutal, is a fast-acting barbiturate medication that functions as a potent central nervous system depressant. First synthesized in the 1930s, this pharmaceutical compound belongs to the barbiturate class of drugs that were once widely prescribed but have since been largely replaced by safer alternatives such as benzodiazepines. Despite this transition in medical practice, pentobarbital continues to serve specific and important roles in human medicine, veterinary practice, and certain legal contexts.
Historical Context and Development of Pentobarbital
Barbiturates were among the first effective sedative-hypnotic medications developed in the early 20th century. Pentobarbital was introduced in 1930 and quickly became popular for its reliable sedative and anticonvulsant properties. Throughout the mid-20th century, it was widely prescribed for anxiety, insomnia, and seizure disorders.
However, as medical understanding of these drugs evolved, significant concerns emerged regarding their narrow therapeutic window, high potential for dependence, and dangerous interactions with other substances, particularly alcohol. By the 1970s and 1980s, benzodiazepines had largely supplanted barbiturates for most indications due to their superior safety profile.
How Pentobarbital Works: Mechanism of Action
Pentobarbital exerts its effects by enhancing the activity of gamma-aminobutyric acid (GABA), the primary inhibitory neurotransmitter in the central nervous system. It binds to GABA-A receptors at sites distinct from benzodiazepine binding locations, prolonging the opening of chloride ion channels.
This action results in neuronal hyperpolarization, making neurons less likely to fire and producing the drug’s characteristic sedative, hypnotic, and anticonvulsant effects. At higher doses, pentobarbital can directly activate GABA-A receptors even in the absence of GABA, which contributes to its potency but also increases overdose risk.
Key Point: Unlike benzodiazepines, pentobarbital can directly activate GABA receptors, making it more potent but also more dangerous in overdose situations.
Medical Applications in Human Healthcare
Pentobarbital maintains several important clinical applications despite the availability of newer medications. Understanding these uses helps clarify why this medication remains relevant in modern medical practice.
Emergency Seizure Control
In emergency neurology, pentobarbital serves as a critical intervention for status epilepticus—a life-threatening condition of prolonged seizure activity that doesn’t respond to first-line anticonvulsant medications. When benzodiazepines and other agents fail to control seizures, pentobarbital may be administered intravenously to suppress excessive neuronal activity.
Procedural Sedation
In perioperative settings, pentobarbital can be used for procedural sedation, helping patients achieve a calm, drowsy state before surgical interventions or anxiety-inducing diagnostic procedures such as:
- Magnetic resonance imaging (MRI)
- Computed tomography (CT) scans
- Minor surgical procedures
- Pediatric examinations
This is particularly valuable for pediatric patients or individuals who experience severe claustrophobia or anxiety during medical procedures.
Induced Therapeutic Coma
One of pentobarbital’s most critical contemporary applications is in neurocritical care, where it is used to induce therapeutic or barbiturate comas in patients with:
- Severe traumatic brain injury
- Refractory intracranial hypertension
- Certain types of brain swelling
By dramatically reducing cerebral metabolic rate and blood flow, high-dose pentobarbital decreases intracranial pressure, potentially preventing secondary brain injury. This intervention is typically reserved for cases where conventional treatments have proven inadequate and is conducted under intensive monitoring in specialized intensive care units.
Historical Use for Insomnia
Historically, pentobarbital was commonly prescribed as a hypnotic agent for insomnia treatment. However, this practice has become extremely rare in modern medicine due to the drug’s significant drawbacks, including:
- Rapid development of tolerance (often within two weeks of regular use)
- High potential for physical and psychological dependence
- Severe withdrawal syndrome
- Narrow margin between therapeutic and toxic doses
Veterinary Medicine Applications
In veterinary practice, pentobarbital serves two primary functions that remain important despite advances in veterinary pharmacology.
Animal Anesthesia
Pentobarbital is employed as an injectable general anesthetic for short-duration procedures in various animal species, particularly small animals such as:
- Dogs and cats
- Rabbits
- Laboratory rodents (mice, rats, guinea pigs)
Its rapid onset and predictable duration make it suitable for minor surgical procedures, though newer anesthetic agents have increasingly replaced it for this purpose.
Humane Euthanasia
More significantly, pentobarbital sodium is considered the gold standard pharmaceutical agent for humane euthanasie in companion animals and laboratory animals. When administered intravenously at appropriate doses, it induces rapid unconsciousness followed by respiratory and cardiac arrest, typically within minutes.
This method is generally regarded as painless and dignified when performed properly by trained veterinary professionals. The American Veterinary Medical Association recognizes pentobarbital as an acceptable euthanasia agent for most animal species.
Forensic and End-of-Life Applications
Pentobarbital has controversial applications in legal execution and end-of-life care that warrant careful, objective examination.
Capital Punishment
In the United States, several states have adopted pentobarbital as part of their lethal injection protocols for capital punishment, particularly as other drugs traditionally used in executions became difficult to obtain due to manufacturer restrictions and international pressure. The drug is typically administered in extremely high doses as part of a single-drug or multi-drug protocol.
Medical Aid in Dying
In jurisdictions where medical aid in dying (physician-assisted suicide or voluntary euthanasia) is legal—including several U.S. states, Canada, parts of Europe, and other countries—pentobarbital may be prescribed to terminally ill patients who meet specific legal criteria.
It is usually provided as a concentrated liquid solution that, when consumed, induces rapid unconsciousness followed by respiratory depression and death, typically within minutes to hours. This application remains legally, ethically, and religiously contentious, with strongly held views on all sides of the debate.
Important Note: The use of pentobarbital in end-of-life contexts is only legal in specific jurisdictions with strict regulatory oversight and qualifying criteria.
Pharmacokinetics and Administration Routes
Understanding how pentobarbital is absorbed, distributed, metabolized, and eliminated is essential for safe clinical use.
Administration Routes
Pentobarbital can be administered through various routes, each with distinct onset times:
- Intravenous (IV): Effects within 1 minute
- Intramuscular (IM): Effects within 10-15 minutes
- Oral: Effects within 15-60 minutes
- Rectal: Effects within 15-30 minutes
Distribution and Metabolism
The drug is rapidly distributed throughout body tissues, crosses the blood-brain barrier efficiently, and has a relatively short elimination half-life of approximately 15-50 hours, though this varies based on individual factors and dosing.
Pentobarbital is primarily metabolized in the liver through oxidation and conjugation reactions, with metabolites excreted through the kidneys. Factors that can significantly affect pentobarbital’s pharmacokinetics include:
- Liver function status
- Patient age (elderly and pediatric populations)
- Concurrent medications
- Chronic use patterns
Safety Concerns and Controlled Substance Status
The safety profile of pentobarbital presents significant concerns that have led to strict regulatory controls worldwide.
Regulatory Classification
The United States Drug Enforcement Administration classifies pentobarbital as a Schedule II controlled substance under the Controlled Substances Act, indicating recognized medical utility combined with high potential for abuse and severe risk of psychological or physical dependence. Similar regulatory restrictions exist in most countries worldwide.
Major Safety Risks
Overdose Potential
Pentobarbital overdose can be fatal, with death typically resulting from profound respiratory depression leading to respiratory arrest, hypoxia, and cardiac arrest. The margin between therapeutic doses and potentially lethal doses is relatively narrow compared to modern sedative-hypnotics.
Tolerance Development
Tolerance develops rapidly with regular use, often requiring escalating doses to achieve the same effects, which increases overdose risk significantly.
Physical Dependence
Physical dependence can develop within weeks of regular use, and abrupt discontinuation can precipitate dangerous withdrawal symptoms including:
- Seizures (potentially life-threatening)
- Severe anxiety and agitation
- Tremors
- Hallucinations
- Delirium
- Cardiovascular instability
Cognitive and Motor Impairment
The drug produces significant cognitive and motor impairment, increasing risks of accidents and falls. Long-term use has been associated with cognitive impairment, mood disturbances, and reduced quality of life.
Dangerous Drug Interactions
Pentobarbital interacts dangerously with alcohol and other central nervous system depressants, potentially causing life-threatening respiratory depression.
Drug Interactions and Contraindications
Pentobarbital interacts with numerous medications through various mechanisms, requiring careful consideration before prescribing.
Enzyme Induction Effects
Pentobarbital is a potent inducer of hepatic cytochrome P450 enzymes, particularly CYP3A4, which can significantly reduce the effectiveness of many drugs metabolized through these pathways, including:
- Oral contraceptives (reducing contraceptive efficacy)
- Anticoagulants (warfarin, requiring dose adjustments)
- Corticostéroïdes
- Certain antibiotics
- Immunosuppressants
- Antifungal medications
CNS Depressant Interactions
Concurrent use with other central nervous system depressants creates additive or synergistic effects that dramatically increase the risk of:
- Profound sedation
- Respiratory depression
- Coma
- Death
Particularly dangerous combinations include pentobarbital with:
- Alcohol
- Opioid analgesics
- Benzodiazepines
- Certain antihistamines
- Muscle relaxants
Absolute Contraindications
Pentobarbital is contraindicated in patients with:
- Severe respiratory disease (COPD, severe asthma)
- Porphyria (a group of rare metabolic disorders)
- Severe liver impairment
- Known hypersensitivity to barbiturates
Use with Caution
Pentobarbital should be used with extreme caution, if at all, in patients with:
- History of substance abuse or addiction
- Depression with suicidal ideation
- Advanced age (elderly patients more sensitive to effects)
- Renal impairment
- Pregnancy or breastfeeding
Signs of Overdose and Emergency Response
Pentobarbital overdose constitutes a medical emergency requiring immediate intervention. Recognition of overdose symptoms can be lifesaving.
Overdose Symptoms
Signs and symptoms of pentobarbital overdose include:
- Extreme drowsiness progressing to unresponsiveness
- Severely slowed or absent breathing (respiratory depression)
- Weak or absent pulse
- Profoundly low blood pressure (hypotension)
- Cold and clammy skin
- Bluish discoloration of lips or fingertips (cyanosis)
- Constricted pupils
- Loss of reflexes
- Hypothermia
- Shock
Emergency Treatment Protocols
Emergency treatment typically involves:
- Airway management: Ensuring open airway and mechanical ventilation support
- Activated charcoal: If the drug was taken orally within 1-2 hours
- Intravenous fluids: To support blood pressure and circulation
- Urinary alkalinization: To enhance drug elimination through kidneys
- Hemodialysis or hemoperfusion: In severe cases to remove drug from circulation
- Supportive care: Temperature regulation, cardiac monitoring
Critical Warning: Unlike opioid overdoses, there is no specific reversal agent (antidote) for barbiturate overdose. Immediate medical attention is essential. Call emergency services (911 in the US) immediately if overdose is suspected.
Current Medical Perspectives on Pentobarbital
Contemporary medical practice views pentobarbital as a medication with limited but important niche applications.
Clinical Positioning
The medical community generally considers pentobarbital a second-line or last-resort option for most indications, reserving its use for situations where safer alternatives have proven inadequate or inappropriate. Ongoing medical education emphasizes the risks associated with barbiturates and promotes familiarity with safer therapeutic alternatives.
Ongoing Research
Research continues into pentobarbital’s role in neurocritical care, though studies have produced mixed results regarding improved outcomes in traumatic brain injury patients treated with barbiturate comas. The medication remains an important tool in the emergency management of refractory seizures, though protocols typically position it after multiple other interventions have been attempted.
Ethical Considerations
The ethical debates surrounding pentobarbital’s use in capital punishment and medical aid in dying continue to evolve, reflecting broader societal discussions about:
- End-of-life autonomy and patient rights
- Capital punishment ethics
- The role of medical professionals in end-of-life decisions
- Regulatory oversight and safeguards
Alternative Medications
For most conditions previously treated with pentobarbital, safer alternatives now exist:
- For anxiety: Benzodiazepines, SSRIs, SNRIs
- For insomnia: Non-benzodiazepine hypnotics (z-drugs), melatonin agonists
- For seizures: Modern anticonvulsants (levetiracetam, valproate, phenytoin)
- For procedural sedation: Propofol, midazolam, dexmedetomidine
Conclusion: Pentobarbital’s Role in Modern Medicine
Pentobarbital represents a pharmaceutical agent with a complex legacy—once celebrated as a medical breakthrough, later recognized for significant risks, and now carefully reserved for specific situations where its unique properties provide therapeutic value that outweighs its considerable dangers.
Its continued use in emergency neurology, neurocritical care, veterinary medicine, and end-of-life contexts underscores that even medications largely supplanted by safer alternatives may retain important clinical roles. However, the stringent regulatory controls, careful medical supervision requirements, and emphasis on alternative treatments reflect the medical community’s recognition that pentobarbital must be approached with appropriate caution and respect for its potent effects on the central nervous system.
Healthcare providers must balance the medication’s legitimate therapeutic applications against its substantial risks, always prioritizing patient safety and considering safer alternatives whenever possible. For patients and the public, understanding pentobarbital’s proper role in modern medicine helps contextualize why this medication remains available despite its dangers, and underscores the importance of using it only under appropriate medical supervision.
Frequently Asked Questions About Pentobarbital
What is pentobarbital used for today?
Pentobarbital is primarily used for emergency seizure control (status epilepticus), inducing therapeutic comas in brain injury patients, procedural sedation, veterinary anesthesia and euthanasia, and in jurisdictions where legal, for medical aid in dying and capital punishment.
Is pentobarbital dangerous?
Yes, pentobarbital is considered dangerous due to its narrow therapeutic window, high potential for overdose, rapid tolerance development, severe withdrawal symptoms, and dangerous interactions with other central nervous system depressants. It is classified as a Schedule II controlled substance.
Why was pentobarbital replaced by other medications?
Pentobarbital was largely replaced by benzodiazepines and other medications because these alternatives have superior safety profiles, wider therapeutic windows, lower overdose risk, and reduced potential for dependence and dangerous drug interactions.
Can you survive a pentobarbital overdose?
Survival from pentobarbital overdose is possible with immediate medical intervention including airway management, mechanical ventilation, and supportive care. However, there is no specific antidote, making prompt emergency treatment critical. Severe overdoses can be fatal.
How long does pentobarbital stay in your system?
Pentobarbital has an elimination half-life of approximately 15-50 hours, meaning it can be detected in the body for several days after administration. The exact duration depends on factors including dose, liver function, age, and individual metabolism.
Medical Disclaimer
This article is for informational purposes only and does not constitute medical advice. Pentobarbital is a potent controlled substance that should only be used under the direct supervision of qualified healthcare professionals. Never attempt to obtain or use pentobarbital without proper medical authorization and supervision. If you have questions about medications, treatments, or health conditions, consult with a licensed healthcare provider. In case of emergency or suspected overdose, call emergency services immediately.